Difference between revisions of "Basic Charge Setup"
Jerri.cowper (talk | contribs) |
Jerri.cowper (talk | contribs) |
||
| Line 90: | Line 90: | ||
=== Charge User Preferences === | === Charge User Preferences === | ||
These preferences are set at the user level. | These preferences are set at the user level. | ||
| − | * Medcin Synonym Search Turned On: Yes or No | + | * [[Medcin Synonym Search]] Turned On: Yes or No |
* Compliance Code Default Entry: GE or GC; specify which modifier will default for the user | * Compliance Code Default Entry: GE or GC; specify which modifier will default for the user | ||
* Compliance Code Required: Yes or No; for use with Resident Physicians | * Compliance Code Required: Yes or No; for use with Resident Physicians | ||
Revision as of 19:59, 29 November 2010
Dictionary Setup
- ICD9 Diagnosis - this dictionary is used to populate all codes available in the Diagnosis tab of the charge workspace; typically loaded from the organizations practice management system; organization has the ability to change the Display Name
- Charge Code - this dictionary is used to populate all codes available in the Procedure AND Visit tabs of the charge workspace; it is recommended that customers keep this dictionary synchronized with their billing systems for item or service charges that the providers may use
- CPT4 Modifier - this dictionary is used to populate the 2-digit codes that can be added to CPT charge codes in order to indicate a service was changed. Modifiers are applicable to either visit, procedure or both.
- Billing Location - this dictionary can be used to populate the location dropdown in the Encounter tab of the charge orkspace (depending on your PM this could be the place of service, ie: office, inpatient)
- Billing Area - this dictionary can be used to populate the location dropdown in the Encounter tab of the charge workspace (depending on your PM this could be the facility location/address)
- Division - this dictionary can be used to populate the division dropdown in the Encounter tab of the charge workspace (depending on your PM this could be the specialty)
- Encounter Type - where individual encounter types are added/edited. If charges are going to be placed against a particular encounter type, within the encounter type dictionary, the following checkbox must be selected: "Can submit charges for the encounter type"
TWUserAdmin Setup
- TWUserAdmin - this is used to determine what providers are available in the Billing Provider and Performing provider dropdown.
-User/Providers marked as Schedulable will be available in the Performing provider dropdown
-User/Providers marked as Billing Provider will be availabe in the Billing Provider dropdown
ChargeAdmin Setup
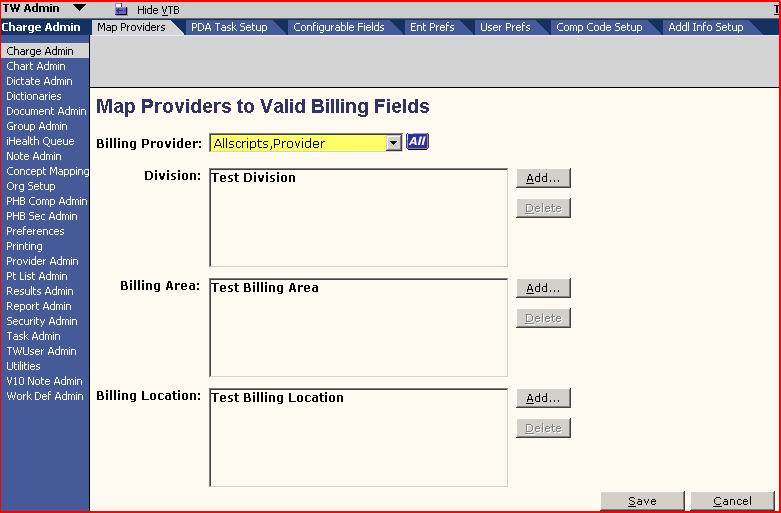
- Charge Admin - this is where the Location, Billing Area, and Division available to each Billing provider is determined/mapped. It is also where some Enterprise preferences are managed as well as additional information fields added
GroupAdmin Setup
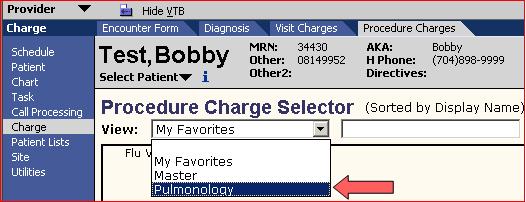
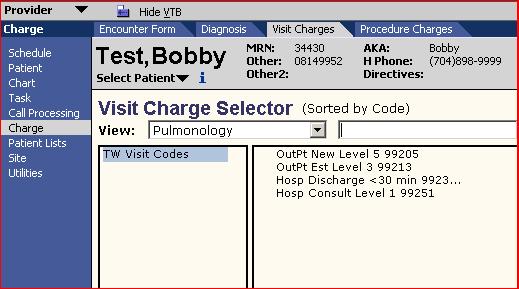
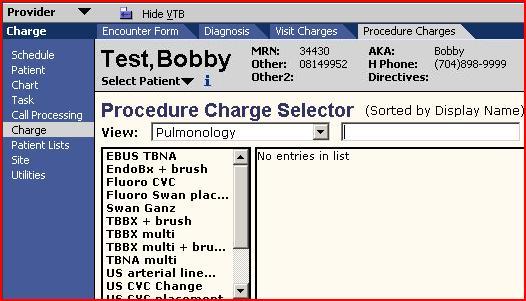
- Group Admin - this is where Groups, Subgroups, and Exploding sets are managed. Groups can be utilized to load group favorites for different specialties. Groups in v10 can be used as specialties are used in v11.
![]()
Groups - Groups can be in the charge workspace by selecting the dropdown found under each of the three tabs: Diagnosis, Visit, Procedure.
Subgroups - Sub-groups can be used for diagnoses, orderable items, procedures, and visit charges, and are typically defined based on anatomy and/or organ system.
Exploding Sets - Exploding sets allow the user to add multiple diagnoses, visit charges, or procedure charges with a single click or tap. This can significantly reduce physician coding time while simultaneously enforcing billing compliance. Exploding sets are most useful for visit types or procedures that are commonly used and where the same diagnoses and/or charge codes are always used together.
Charge Encounter Types
The following are encounter types that you will see during the course of charge related workflows, also corresponding tasks you may see with these encounters.
- Appointment Encounters:
Data will be populated from appointment: billing provider, performing provider, referring provider (if available), billing area, and location
Related submission tasks: Submit Enc Form, Review Enc Form
- Result Charge Encounters:
If the encounter is not linked to an appointment charge module displays the day and date of the encounter. Billing provider may be populated from the orderable item. You may select performing provider, referring provider, division, billing area, and location.
Related submission tasks: Submit Res Enc, Review Enc Form
- Non-appointment Encounters:
If the encounter is not linked to an appointment, the charge module displays the day and date of the encounter. You can select the billing provider, performing provider, referring provider, division, billing area, and location.
Related submission tasks: Submit Enc Form, Review Enc Form
- Inpatient encounters:
If the encounter is related to an inpatient stay, the charge module displays the day, date, and room/unit number. Billing provider will default. You can select the performing provider, referring provider, division, billing area, and location.
Related submission tasks: Submit IP Form, Review Enc Form
Charge Encounter Submission Status
- Not Submitted – encounter has not yet been submitted.
Task: Submit Enc Form, Submit IP Enc, Submit Res Enc - Review – provider has completed initial submit, waiting on Final Submit.
Task: Review Enc Form - Ready - user that has final submit priveleges has clicked submit, but encounter form is not ready for submission - for example - a local patient has not been merged.
Task: Review Enc Form - Submitted – encounter has been submitted, items are in a status of Submitted and charge is waiting on PM import.
Task: no outstanding charge tasks - Edited – user that has final submit privileges has submitted charges. Charge is waiting on PM import and an item on the encounter is edited.
Task: Adjust Charges
Charge Related Preferences
Enterprise-Level Charge Preferences
- CCI Edit Checking Turned On—Indicates that CCI edit checking is enabled; select Yes or No.
- RVU Type to Display—Indicates the RVU type to display during CCI edit checking; select Facility or Non-Facility.
- 25 Modifier Checking Turned On—Indicates that 25 Modifier Checking functionality is enabled; select Yes or No.
- Free Text Referring Provider Turned On—Indicates that users can enter a free text referring provider in the application; select Yes or No.
- Non-billable Diagnosis Code Checking Turned On—Indicates how non-billable diagnosis codes are utilized in the system. Select one of the following:
- No—Non-billable diagnosis code checking is turned off
- Non-billable codes selectable—Users can select nonbillable diagnosis codes, and the system displays the appropriate indicator
- Non-billable codes not selectable—The system displays non-billable diagnosis codes (in gray, italicized text), but users cannot select them.
- Medcin Synonym Search Turned On—Indicates the Medcin synonym search on the (ICD9) Diagnosis selector window in the Web and the PDA applications in connected mode is enabled. Select Yes or No.
- Compliance Code Field Turned On—Select Yes to display compliance code-related data on the Encounter Form pages and screens.
- Compliance Code Default Entry—Select a default compliance code for new users; if a Compliance Code dictionary entry is not selected, then the system does not display a default entry for new users.
- Compliance Code Required—Select Yes if the user must select a compliance code for an encounter before it can be submitted for billing.
- Medical Necessity Checking Turned On—Default value is N (no). Set to Y (yes) to have the system perform Medical Necessity Checking.
- Hold charges for ABN Status—If Yes, then charges that fail Medical Necessity Checking have Billing Status of Needs Info until the ABN Status is entered; if No, then charges that fail Medical Necessity Checking are submitted if no other edits exist.
- ABN Status Modifier: Patient signed the ABN and accepts financial responsibility— Select the appropriate entry from the CPT4 Modifier dictionary; that modifier is added to the charge for which the ABN Status was entered.
- ABN Status Modifier: Patient signed the ABN and does not accept financial responsibility—Select the appropriate entry from the CPT4 Modifier dictionary; that modifier is added to the charge for which the ABN Status was entered.
- ABN Status Modifier: Patient refuses to sign the ABN—Select the appropriate entry from the CPT4 Modifier dictionary; that modifier is added to the charge for which the ABN Status was entered.
- ABN Status Modifier: ABN not obtained—Select the appropriate entry from the CPT4 Modifier dictionary; that modifier is added to the charge for which the ABN Status was entered.
- Encounter Locking Turned On—Indicates if Encounter Locking is enabled; select Yes or No.
- Encounter Lock Timeout (Days)—Indicates the number of days until which the encounter lock timeout occurs. Enter a number (of days).
- Submit All Charges When Ready Turned On—Indicates if the system automatically submits charges when they are ready; select Yes or No.
- Hierarchical Condition Category (HCC) Checking Turned On—Allscripts contracts with 3M Health Information Systems to obtain HCC diagnoses data. This data is passed to clients through the Delta process. To configure the TouchWorks system to display HCC indicators throughout the Charge module, select Yes.
Charge User Preferences
These preferences are set at the user level.
- Medcin Synonym Search Turned On: Yes or No
- Compliance Code Default Entry: GE or GC; specify which modifier will default for the user
- Compliance Code Required: Yes or No; for use with Resident Physicians
Charge Related Tasks
| Task Name: | Module: | Is created by: | When: | And the Task Action is: | And assigned to: | And is resolved: | Is the task delegated? | |
| ABN Follow-up | Charge | The system | A procedure charge is deemed medically not necessary and activated when the system preference Hold charges that fail medical necessity checking = No. System generated if a charge fails medical necessity checking. | Process Encounter | Billing provider | Manually completed when charges are edited in the practice manage system, and the user clicks Done. Auto-completed if charge is edited to pass medical necessity checking. | No | |
| Go To Enc Form | Charge | A user | A user clicks New Task on the Encounter Form page and indicates Go To Enc Form in the Task box or a follow-up task is created on the PDA. | Go To Enc Form | User specified on the Encounter Form New Task page | Manually completed when the user clicks Done. | No | |
| Adjust Charges | Charge | The system | A user edits or removes charges that have already been sent to billing. | Process Encounter | Billing provider | Manually completed when the charges are edited in the practice management system, and the user clicks Done. | No | |
| Submit Enc Form | Charge | The system | An arrived appointment is received by the system or when additional charges added to encounter without resubmitting encounter form. | Send Charges | Billing provider; if none, then appointment provider; if none, then Encounter Followup Team | Auto-completed when: 1. User clicks Submit regardless of the status of any change on that encounter. 2. User cancels a charge and the rules for creating a Submit Enc form task fail and there are no charges with a status of Needs Info, Saved, or Ready. | No | |
| Review Enc Form | Charge | The system | Created for coders and attending physicians to review the encounter forms submitted by specified providers before charges are submitted to the practice management system for billing. System generated when a user clicks or taps Submit and based on the ChgWorksCreateRevEncFormTasks user preference which is set in Admin (not in the Personalize Charge page). | Review Charges | Enc Review team | Auto-completed when all charges on the encounter are submitted by a user without the ChgWorksCreateRevEncFormTasks user preference. | No | |
| Injury/WC F/up | Charge | The system | Created when injury information is deemed necessary for a selected diagnosis. Activated when the system preference CWWorksPrefCreateInjTask = Y. System generated if the system option set to create and special billing condition is entered on the encounter form. | Process Encounter | Enc Review team | Manually completed when charges are edited in the practice management system, and user clicks Done. | No | |
| Mng Chg Edits | Charge | The system | If there are one or more charges on the encounter with the status of Needs Info. | Edit Charges | Charge Edits Team | Automatically completed when there are no charges on the encounter with status of Needs Info. | No | |
| Submit IP Enc | Charge | The system | System generated according to the preference on the service list and if an inpatient encounter form has charges on it that are not submitted and there is no Submit IP Enc task. | Send Charges | Billing provider | Auto-completed when: 1. User clicks Submit regardless of the status of any change on that encounter. 2. User cancels a charge and the rules for creating a Submit IP Enc task fail and there are no charges with a status of Needs Info, Saved, or Ready. | No | |
| Submit Res Enc | Charge | The system | System generated if a Submit Enc Form task does not exist for that Result Charge encounter. There cannot be an active Submit Enc Form task and an active Submit Res Enc task on the same encounter. | Send Charges | Lab Charges Team | Auto-completed when: 1. User clicks Submit regardless of the status of any change on that encounter. 2. User cancels a charge and the rules for creating a Submit Res Enc task fail and there are no charges with a status of Needs Info, Saved, or Ready. | No | |
| Print Enc Form | Charge | The system | Through the encounter form automatic printing set-up, this task is created when all charges are submitted and reach a status of Submitted or Review. System generated if system option is set to create and all charges are either (1) Submitted or (2) Submitted or Review. | Print Enc Form | Billing provider | Auto-completed when the encounter form is printed. | No | |
Basic Charge Workflows
- Basic Ambulatory Charges—Used to submit charges for an ambulatory visit when Note is not used.
- Charging from Note—Used to submit charges after creating a Note.
- Charging for Orders—Used to submit charges for a billable orderable item.
- Charging for Administration—Used to submit charges for a billable medication/immunization administration, as well as any associated supplies used for that administration.
- Review Encounter Charges—Used by billing staff to review submitted charges prior to sending to an organization's Practice Management System.