Difference between revisions of "Charge Questions/Answers"
Kavon.Kaboli (talk | contribs) |
Kavon.Kaboli (talk | contribs) |
||
| Line 48: | Line 48: | ||
'''A:''' The use of the G-Code is going to be very specific to your particular organization, your Charge module configuration and the workflows you already have in place with the providers. Make your G-Code available for use on the Encounter Form as they are needed not only in the documentation process, but also with charge submission. Proper involvement of the coding office and educational services will be needed. Depending on how you have set up your charge review process, someone in the Billing Office may be able to assist the providers with reviewing the Encounter Forms prior to submission or use of a TES edit is always something to investigate, if that software is available to your organization. Of course, in the end, it is the providers’ responsibility to ensure all submitted claims meet carrier requirements. Do your reading and research on the Medicare requirements and as we stated during the presentation….test, test and test some more! | '''A:''' The use of the G-Code is going to be very specific to your particular organization, your Charge module configuration and the workflows you already have in place with the providers. Make your G-Code available for use on the Encounter Form as they are needed not only in the documentation process, but also with charge submission. Proper involvement of the coding office and educational services will be needed. Depending on how you have set up your charge review process, someone in the Billing Office may be able to assist the providers with reviewing the Encounter Forms prior to submission or use of a TES edit is always something to investigate, if that software is available to your organization. Of course, in the end, it is the providers’ responsibility to ensure all submitted claims meet carrier requirements. Do your reading and research on the Medicare requirements and as we stated during the presentation….test, test and test some more! | ||
| + | |||
'''Q:''' Any recommendations on handling self-pay processes? | '''Q:''' Any recommendations on handling self-pay processes? | ||
Revision as of 20:13, 4 September 2013
Q: How does the Free Text Referring Physician field work within the Encounter?
A: When a provider selects a consult code and they are unable to find the referring physician they can type in the search box, click the "misc" button and click "ok". This adds what the provider entered in the search box as a free text referring physician. When the provider submits the charge a "Mng Chg Edits" task is created for the Charge Edits Team. When the Charge Edits team opens the task it takes them to the encounter where there is the red frowny face that tells them there is a free text referring physician. They then research and add the referring physician in Practice Management System if necessary, then go into the EHR and select the now selectable referring physician and click submit.
- Please note this is an Enterprise Preference and can be set under the Charge Admin tab. Many organizations choose to set this preference to NO due to billing issues that may arise if the correct referring provider is not indicated on the encounter.
Q: When the front desk arrives an appointment in error, then subsequently cancels the same appointment in the Practice Management system, what happens to the "Submit Enc Form" task?
A: Once the appointment is cancelled in the Practice Management system the task should resolve itself.
Q: I realize the $ in the daily schedule means the charge was submitted, & in the clinical desktop, there is a blue check mark that means the charge was submitted to our practice mgmt system...is it possible to have the blue check mark show on daily schedule?
A: I’m not aware of any method by which you could get the blue check mark to show on the daily schedule unfortunately. My suggestion would be to enter a case with Support Force. It might be that this is billable customization work that Allscripts would do for your organization. However, my initial thought is that it is not.
Q: Can the date of service be a header in the task view? Currently, you can't see the date of encounter until you click on a task and view the ""task about"" box at the bottom left of the screen. Date of service as a header would save a HUGE amount of time!!!
A: I’ve never seen any documentation that would indicate DOS could be utilized as one of the headers in the task view. However, the created on date, should be the date that the appointment was arrived at least for the “Submit Enc Form” tasks. Of course, once those initial tasks are resolved by your providers and a “Review Enc Form” or “Mng Chg Edits” task is kicked off, that logic will no longer be applicable. I completely agree it would make back office workflows much smoother if that DOS info was contained in the task. It’s as if development just stopped one step shy of a great idea. However, if you’ve got someone in your organization that’s really handy with SQL and knows the DB tables, it may be that a custom report would fit your needs better than a task list anyway. The drawback there would be that you would have to manually pull each of those patients into context.
Q: Is the Charge module required for Meaningful Use?
A: Originally, yes. Use of the Charge module was going to be required to complete Meaningful Use reporting in Stage 1. However, I believe there were changes made to that approach after the picture became a little clearer around MU and the amount of work that was going to be required was better understood. At that point, the shift was made to utilizing the Data Mapping workbook to indicate the “encounters” that should be used to calculate individual measures. However, I had seen a more recent discussion on Client Connect concerning possible requirements in future MU Stages at (https://clientconnect.allscripts.com/thread/15337?tstart=0) . It may be worthwhile to follow up with the discussion if you have further questions Allscripts could address.
Questions from presentation on 8/16/13
Q: ABN workflow?
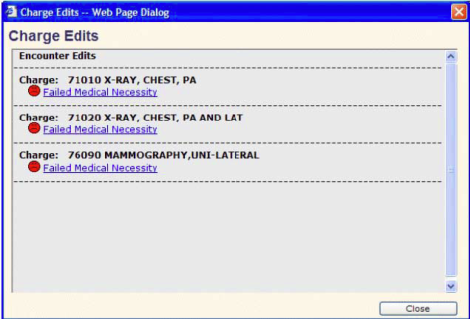
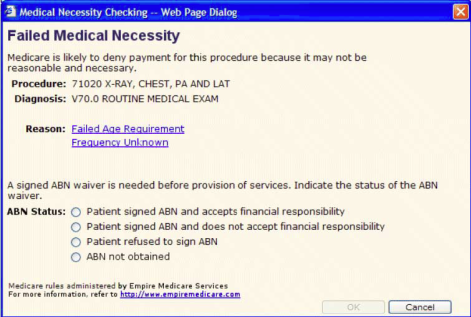
A: Please note, the physician is advised as to whether an Advance Beneficiary Notice (ABN) needs to be obtained before services are rendered. Medical Necessity Checking automatically occurs in the background as charges are saved for an encounter involving a specially insured patient. When a charge is flagged as not medically necessary, either a red or yellow face will display for the specified charges on the encounter form. Note: Depending on whether the Hold ABN Status preference is set to Yes or No, the icons next to the edit links are displayed in red or yellow. Red indicates that the edit must be resolved before the encounter can be submitted. Yellow indicates that it is recommended that the edit be resolved, but the charge(s) can be submitted without it. Charges for Medicare patients are checked for medical necessity and edits are accessible from the Encounter Form page. Charges that fail medical necessity can be held until the advance beneficiary notification (ABN) status is entered. Appropriate modifiers can be appended to the failed charges so that when they are sent to the billing system, they appear correctly on the claim form.
With all that being said, the ideal ABN workflow would include system configuration that prompts the provider that Medical Necessity has been failed and at that point the patient can discuss the need for ordered services and/or other available options directly with the provider and sign the ABN or decline the service in question. The documentation can then be scanned to the patients chart as appropriate for your organization. However, my personal experience has been that many providers do not feel overly comfortable with this process. If that’s the situation you are dealing with, this is definitely a discussion that needs to take place with Management, providers, billing office personnel and whomever in your organization is in charge of pre-authorization processes.
Q: G-code workflow? Recommended?
A: The use of the G-Code is going to be very specific to your particular organization, your Charge module configuration and the workflows you already have in place with the providers. Make your G-Code available for use on the Encounter Form as they are needed not only in the documentation process, but also with charge submission. Proper involvement of the coding office and educational services will be needed. Depending on how you have set up your charge review process, someone in the Billing Office may be able to assist the providers with reviewing the Encounter Forms prior to submission or use of a TES edit is always something to investigate, if that software is available to your organization. Of course, in the end, it is the providers’ responsibility to ensure all submitted claims meet carrier requirements. Do your reading and research on the Medicare requirements and as we stated during the presentation….test, test and test some more!
Q: Any recommendations on handling self-pay processes?
A: I’m sure there are quite a few options out there, but what I’ve personally used is the Discount Type workflow discussed in the presentation. Kavon referred to Clergy and Professional Courtesy dictionary entries in the webcast. That dictionary is manually populated and an entry of Self-Pay, Non-Primary Insurance, Workers Comp, Gift Certificates, etc could easily be utilized as well. Some creative mapping with interface messages could allow for those charges to fall out of the normal charge submission workflow and flag these particular encounter forms to be manually worked by the billing staff. And again, testing is going to be key in this process to ensure processing to the patients primary insurance does not occur.
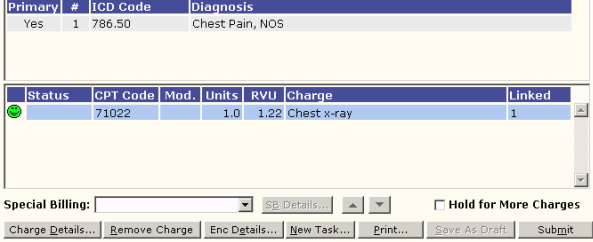
Q: Can you demonstrate what a Discount type would look like on the charge encounter?
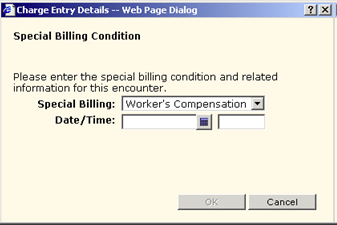
A: The Special Billing field seen below, left can be utilized and depending on your configuration, you can allow for the inclusion of proper supporting information for billing purposes in the Charge Entry Details window seen to the right below. Again, with some proper interface message mapping, the information in question can flow to the Practice Management System for billing.
Q: Where are the things in the discount dictionary applied to the encounter form?
A: Please see the previous question and answer.
Q: Isn't the PM to EMR interface capable of populating some of the fields on the encounter form?
A: Yes! Again, this is going to be dependent on your organizational configuration with the PM and EHR. Given there are so many varieties of configurations that could be in place out there, we didn’t feel comfortable going into this during the presentation. However, work with your interface analyst, know what fields are available for use and test out some mapping options. If your organization doesn’t have an Interface Analyst, or they don’t feel comfortable taking on this challenge, reach out to the Galen team as our Interface Analysts are very adept at this type of work.
Q: Have you set up charging of the EEHR for provider based billing?
A: I have not personally been involved with that specific configuration. However, the Charge module is highly configurable and as long as proper testing is completed prior to implementation, provider based billing should be an option.