Difference between revisions of "Insurance Class"
Steve.Stahr (talk | contribs) (New page: The Insurance Class dictionary contains the various payors associated to a practice. They are commonly the same list of payors found in the PMS. In the EHR dictionary, the key fields to t...) |
|||
| (11 intermediate revisions by 7 users not shown) | |||
| Line 1: | Line 1: | ||
| + | __TOC__ | ||
| + | [[Category:Allscripts_Touchworks_EHR_Dictionaries]] | ||
| + | |||
| + | ==Version Information== | ||
| + | *[[Article Creation|Article Created based on version]]: 11.1.1 | ||
| + | *[[Article Last Update|Last Updated with version]]: | ||
| + | |||
| + | =Description= | ||
| + | |||
The Insurance Class dictionary contains the various payors associated to a practice. They are commonly the same list of payors found in the PMS. | The Insurance Class dictionary contains the various payors associated to a practice. They are commonly the same list of payors found in the PMS. | ||
In the EHR dictionary, the key fields to the Insurance Class entries are Code, Name and Mnemonic. These can be entered manually or bulk-loaded by the implementation and interface team. | In the EHR dictionary, the key fields to the Insurance Class entries are Code, Name and Mnemonic. These can be entered manually or bulk-loaded by the implementation and interface team. | ||
| Line 7: | Line 16: | ||
==Multi-Organization system interfaced with multiple PMS== | ==Multi-Organization system interfaced with multiple PMS== | ||
| − | In this circumstance, each distinct instance of | + | In this circumstance, each distinct instance of the PMS's Insurance Class may either be added '''or''' a standardized Insurance Class dictionary is built and subsequent Organizations/PMS Insurance's are mapped to the standard set of Insurances. |
| + | |||
| + | When mapping insurance classes, two fields are critical - the FSC and the Company ID (HL7 segment IN1, fields 2 & 3). These will uniquely identify the insurance payor and plan in the PMS, allowing the practice to submit claims accurately. Mapping the insurances from the PMS to EMR is a complex process and resources familiar with the codes should be heavily involved in the process. | ||
| + | |||
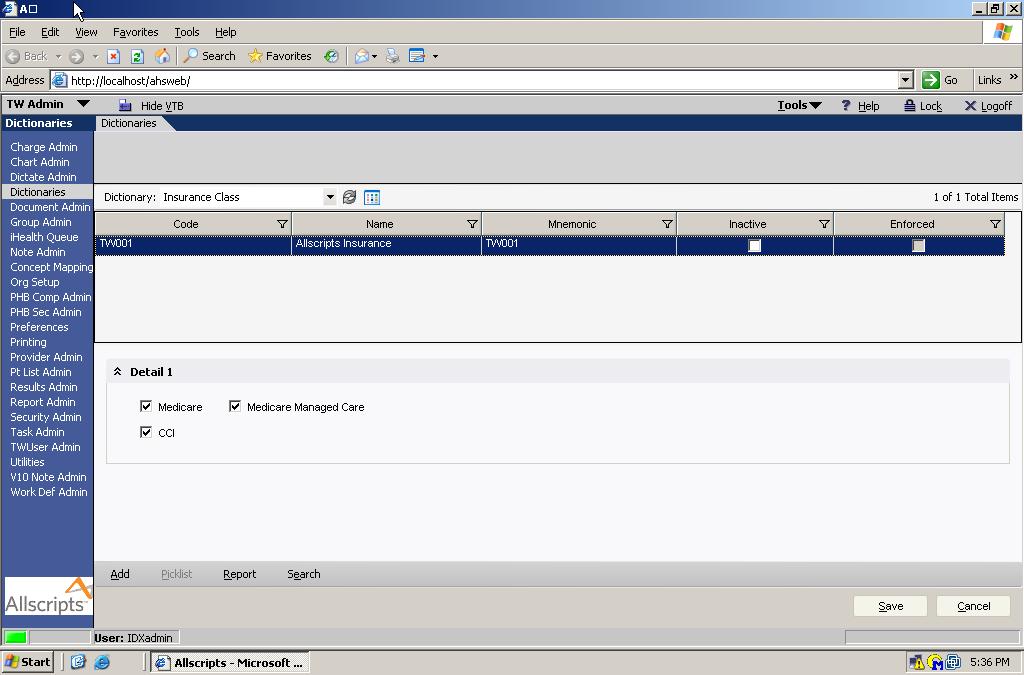
| + | [[Image:Insurance Class1.jpg]] | ||
| + | |||
| + | |||
| + | * '''Code''' - The Code is a unique identifier that must be supplied. This is not displayed in the product and is used for identification purposes only. | ||
| + | * '''Name''' - This is the name that will appear for the end users in the EHR application. This should be unique to prevent confusion. | ||
| + | * '''Mnemonic''' - This is not required, but it used as a secondary identifier. This does not appear in the product and unless you have another use for it, the recommendation would be to make this the same as the code. | ||
| + | * '''Inactive''' - The inactive flag allows you to inactivate or hide an entry. If an item is inactivated, users would not have the ability to select the payor in the future, although any patients with the payor defined would remain viewable. | ||
| + | * '''Enforced''' - The enforced flag designates whether a dictionary item is required and cannot be changed. In most cases, this comes predefined by Allscripts and should not be selected for new entries. If an entry is enforced, it cannot be modified or inactivated. | ||
| + | * '''Medicare''' - this is required in order to take advantage of the ABN feature (medical necessity checking) and any additional information details identified; also used in some order feature sets (setting default requested performing location) | ||
| + | |||
| + | * '''Medicare Managed Care''' - this is required to take advantage of HCC coding and any additional information details identified; also used in some order feature sets (setting default requested performing location) | ||
| + | |||
| + | * '''CCI''' - this is required to identify insurance carriers | ||
| + | |||
| + | ==Purpose of this dictionary in the EHR:== | ||
| + | |||
| + | *HCC Checking | ||
| + | *Medical Necessity Checking | ||
| + | *Prior Authorization for Orders | ||
| + | *Addl Info Setup - example: G Codes for Medicare patients with an E/M code | ||
| + | *Insurance display on Daily Schedule and Patient Demographics (I) screen | ||
| + | *Patient-level information may be sent on outbound interfaces. For example, current insurance information sent to a lab along with orders. | ||
| + | *Insurance display on Daily Schedule and Patient Demographics (I) screen | ||
| + | *Patient-level information may be sent on outbound interfaces. For example, current insurance information sent to a lab along with orders. | ||
Latest revision as of 16:58, 10 November 2016
Version Information
Description
The Insurance Class dictionary contains the various payors associated to a practice. They are commonly the same list of payors found in the PMS. In the EHR dictionary, the key fields to the Insurance Class entries are Code, Name and Mnemonic. These can be entered manually or bulk-loaded by the implementation and interface team. If the SureScripts and/or RxHub (see E-prescribing) functionality is available and deployed, the prescription formularies will be available to providers in the Rx+ module.
Multi-Organization's sharing a single PMS instance
In an environment that shares a common PMS can simply build the Insurance Class dictionary into the EHR, copying the codes, names, and mnemonics.
Multi-Organization system interfaced with multiple PMS
In this circumstance, each distinct instance of the PMS's Insurance Class may either be added or a standardized Insurance Class dictionary is built and subsequent Organizations/PMS Insurance's are mapped to the standard set of Insurances.
When mapping insurance classes, two fields are critical - the FSC and the Company ID (HL7 segment IN1, fields 2 & 3). These will uniquely identify the insurance payor and plan in the PMS, allowing the practice to submit claims accurately. Mapping the insurances from the PMS to EMR is a complex process and resources familiar with the codes should be heavily involved in the process.
- Code - The Code is a unique identifier that must be supplied. This is not displayed in the product and is used for identification purposes only.
- Name - This is the name that will appear for the end users in the EHR application. This should be unique to prevent confusion.
- Mnemonic - This is not required, but it used as a secondary identifier. This does not appear in the product and unless you have another use for it, the recommendation would be to make this the same as the code.
- Inactive - The inactive flag allows you to inactivate or hide an entry. If an item is inactivated, users would not have the ability to select the payor in the future, although any patients with the payor defined would remain viewable.
- Enforced - The enforced flag designates whether a dictionary item is required and cannot be changed. In most cases, this comes predefined by Allscripts and should not be selected for new entries. If an entry is enforced, it cannot be modified or inactivated.
- Medicare - this is required in order to take advantage of the ABN feature (medical necessity checking) and any additional information details identified; also used in some order feature sets (setting default requested performing location)
- Medicare Managed Care - this is required to take advantage of HCC coding and any additional information details identified; also used in some order feature sets (setting default requested performing location)
- CCI - this is required to identify insurance carriers
Purpose of this dictionary in the EHR:
- HCC Checking
- Medical Necessity Checking
- Prior Authorization for Orders
- Addl Info Setup - example: G Codes for Medicare patients with an E/M code
- Insurance display on Daily Schedule and Patient Demographics (I) screen
- Patient-level information may be sent on outbound interfaces. For example, current insurance information sent to a lab along with orders.
- Insurance display on Daily Schedule and Patient Demographics (I) screen
- Patient-level information may be sent on outbound interfaces. For example, current insurance information sent to a lab along with orders.