Rx Hub
RX HUB and Eligibility Checking
Allscripts is providing a new feature in V11 that provides a feed of medication history for patients with PBM Claim history. TouchWorks EHR has been receiving medication history from the PBMs participating in Rx Hub since V10. However, V10 couldn't handle the feed very well so the information was previously blocked.
How It Works
There is an Enterprise setting within TouchWorks that, when turned on, allows PBMs to feed patient medication history through Eligibility Checking. Eligibility checking is a process within Rx Hub that occurs every 30 min and looks for all patients with a scheduled appointment in TouchWorks based on participating PBMs. If any scheduled patient subscribes to a participating PBM, this process will then load any medication that the patient submitted a claim for.
This process contains 18 months of patient history, however there is logic in place to load a patient medication if:
1) The provider is within the organization: it updates the medication list if it doesn’t appear, but won’t make any changes to a refilled medication.
2) If the medication was prescribed by a provider outside of the organization it places the med in a status of Unverified.
3) The logic is smart enough to look for the medication in the patients chart under any status (EIE, Removed, D/C…) and not add to the meds list if that medication already exists under the NDC #. The only time this might not be the case is in when a dosage change is completed in TW as a “Renew w/Changes”. However, this would only occur the first time that the med was loaded.
Additionally, because of the interface between TouchWorks Practice Management and TouchWorks EHR the patient’s appointment will appear in the EHR even if the provider isn’t currently using TouchWorks. Therefore, it’s possible for a patient’s medication history to be populated in the EHR prior to the practice Go Live.
Allscripts is currently blocking the other PBMs participating in Eligibility checking, but we do have the capability of receiving all PBM’s that participate if we choose to. They are:
- Aetna
- Caremark
- Medco
- Argus
- Pharmacare
- ESI
- Wellpoint
We won’t receive plan information from the PBM’s, and certain PBM’s won’t pass sensitive medication history, i.e. HIV drugs or Psych meds. If we turn either the flag to receive the feeds on or remove the filters for the PBM’s, it is set at an Enterprise level.
What happens when a patients medication lists have already been imported into the EHR through this process?
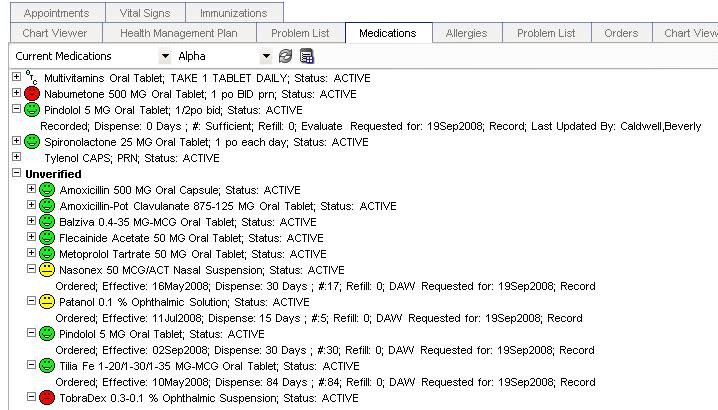
These medications are imported as unverified medications as shown below. The information includes drug name, date, dose, days supply and #pills. It does not include the SIG, because it is claims information only. (See Figure 1)
Figure 1:
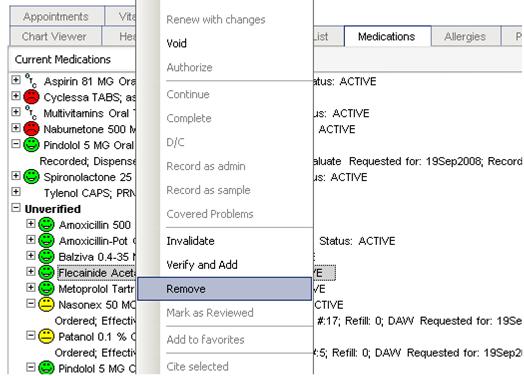
The medication remains in the unverified status until each one is verified by selecting one of three options: Invalidate, Verify and Add, or Remove. This is done through the right-click menu as shown in Figure 2 below.
Figure 2:
Future Plans
Allscripts is currently working with SureScripts and Rx Hub to expand this capability. SureScripts can provide medication history at the pharmacy level; this would be beneficial in cases where an insurance claim wasn’t submitted. They are currently working with Walgreen’s, and it’s in early stages so the capability is by state and only 50% of Walgreen’s patient population.